Understanding your fertility
Men are fertile all the time. Women are fertile for about one third of an average menstrual cycle.8 The woman’s own body gives her signs to help her identify when she is potentially fertile during the cycle.
Fertility Indicators
The signs which the woman can detect herself are called the fertility indicators and include changes in (i) the cervical mucus, (ii) in basal body temperature (BBT) and (iii) in the cervix. These signs and symptoms have a scientific basis and are due to the effects of the ovarian steroid hormones, oestrogen and progesterone, on the fertility indicators during the cycle.6
Fertility Awareness
Fertility awareness means that the woman, by keeping a daily record on a chart of the changes that occur in cervical mucus, in basal body temperature, and in the cervix during the cycle, will be able to identify when the fertile and infertile phases of the cycle occur, irrespective of cycle length.4
Natural family planning (NFP) is when the woman applies the Rules of her chosen method of NFP to this daily record in order to define when the fertile and infertile phases begin and end. The couple must learn these rules from a qualified NFP teacher.
Classification of the Fertility Indicators
The fertility indicators are classified as major indicators which can detect either the beginning or the end of the fertile phase, and minor indicators which are inconstant and do not detect the beginning or the end of the fertile phase.9 The scientific basis for these effects are well described in the study by Moghissi.6
Major Indicators
- Changes in cervical mucus.4
- Changes in basal body temperature (BBT).3
- Changes in the cervix5
Minor Indicators
The woman may also find other fertility indicators of a minor nature useful, such as the ‘calendar calculation’, and the presence of various symptoms (called molimina) e.g. ovulation pain (mittelschmertz)’ or breast symptoms.
When is the fertile phase of the menstrual cycle and how long does it last?
The fertile phase of the cycle includes the time when the mature ovum is available for fertilization at ovulation and the 6 days or so leading up to ovulation when oestrogenic fertile-type cervical mucus is present. (Fig. 7-16).
In other words the fertile phase is the combined time of the lifespan of the ovum (egg) after ovulation, (24 hours), and the lifespan of sperm in fertile-type mucus before ovulation, (5 days).1,2 Therefore the fertile phase during which sexual intercourse could potentially result in conception lasts for 6 – 9 days.7
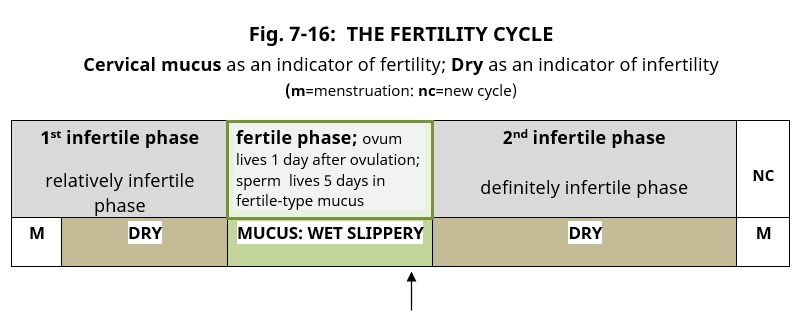
Fig. 7-16 (The fertility Cycle) : This diagram shows the three phases of the fertility cycle, the fertile phase comes after the 1st infertile phase and before the 2nd infertile phase. The presence of mucus at the vulva either by sensation or appearance is an indication of potential fertility. The 2nd infertile phase after ovulation is definitely infertile as the ovum lives for just one day and there will be no further ovulation in that cycle.
Can fertility awareness and natural family planning be used by women with irregular cycles?
All women can use fertility awareness and natural family planning to identify when they are potentially fertile by learning to recognise the changes in the fertility indicators, that is, changes in the ‘cervical mucus’, ‘basal body temperature’, and ‘cervix’ during the cycle, (fertility awareness). This applies to all women of child-bearing age whether their menstrual cycle is regular or irregular.
References
- Wilcox AJ, Weinberg CR, Baird DD; ‘Timing of sexual intercourse in relation to ovulation – effects on the probability of conception, survival of the pregnancy, and sex of the baby’; N Engl J Med 1995; 333;1517-21.
- Simpson JL; Editorial, Pregnancy and the timing of Intercourse; N Engl J Med 1995; 333;1563-64.
- Marshall, J; A field trial of the basal body temperature method of regulating births; Lancet, 1968, July, 8-10;
- Billings, E & J; Symptoms & Hormonal Changes accompanying ovulation; Lancet; Feb5; 1972; 282-284.
- Keefe, E.; ‘Self-observation of the cervix to distinguish days of possible fertility’; Bull of the Sloane Hosp for Women; 1962; 129-136.
- Moghissi KS, Syner FN, Evans TN: ‘A composite picture of the menstrual cycle’; Am J Obstet Gynecol, 1972; 114:405- 418. Commenting on this study by Moghissi, Dr M.L. Taymor, Boston, Massachusetts states on page 416, “The special contribution of this paper is the correlation of the changes in the end-organ responses, i.e. BBT, and changes in cervical mucus, with the hormonal changes. As a result, these changes which are naturally of more interest to the clinician, are placed on a firmer physiologic basis.”
- Freundl G, Godehardt E, Kern PA, et al; “Estimated maximum failure rates of cycle monitors using daily conception probabilities in the menstrual cycle”; Human Reproduction, (2003), vol 18, no. 12, p2628-2633.
- Klaus, Hanna; ‘Natural family planning – Is it scientific? Is it effective?’ page 1; Newman Lecture Series 1; May 21, 2000. (online).
- Flynn A, Brooks M;‘The Manual of Natural Family Planning’;1996; ISBN 0 72253115 X


