What is the menstrual cycle?
What is the Menstrual Cycle
The menstrual cycle is the woman’s reproductive cycle which occurs each month during her child-bearing years, the most obvious sign being menstruation.
The two objectives of the menstrual cycle are (a) development of the immature ovum and (b) development of the lining of the womb (endometrium) :
-
(a) During each menstrual cycle an immature ovum (follicle, egg) develops and is released as a mature ovum into the fallopian tube ready to be fertilized, (ovulation). Ovulation usually occurs about 14 days before the next menstrual period and the ovum lives for 24 hours. See Fig 6-16 page 15 in Pictures & Diagrams
-
(b) The first day of the cycle is the first day of menstruation, and when the menstrual period has finished the lining of the womb (endometrium) starts to regrow again under stimulation from oestrogen before ovulation and progesterone after ovulation. This is to prepare the endometrium for possible pregnancy in order to nourish the fertilized ovum after it has implanted in the uterus. However if pregnancy does not occur the lining of the womb is shed as menstruation about 14 (10-16) days after ovulation, and a new cycle begins.
Details of the menstrual cycle are outlined on diagrams under the following headings:
- The length of the cycle: Fig. 6-1
- The two phases in the menstrual cycle are the follicular phase and the luteal phase: Fig. 6-2
- When does ovulation occur? – are the follicular & luteal phases of the cycle the same length? Fig. 6-3
- Hormone secretion by the growing ovarian follicle and corpus luteum in the ovary during the cycle: Fig. 6-4
- Overview of the phases of the cycle: Fig. 6-5
The length of the cycle, see Fig. 6-1
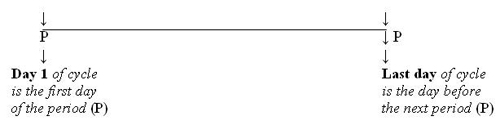
Fig. 6-1; The length of the menstrual cycle: By convention Day 1 of the cycle is the first day of the menstrual period, and the last day of the cycle is the day before the next menstrual period. The length of the cycle can vary from 21-35 days, and is on average 28 days.
The two phases in the cycle, see Fig. 6-2
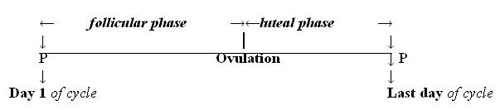
Fig.6-2; The phases of the menstrual cycle: The menstrual cycle is divided into two phases by ovulation (the release of the ovum): (a) the follicular phase when the ovum is maturing before ovulation and (b) the luteal phase after ovulation.
Two Questions: (i) When in the cycle does ovulation occur? (ii) Are the follicular and luteal phases of the cycle equal in length?, see Fig. 6-3
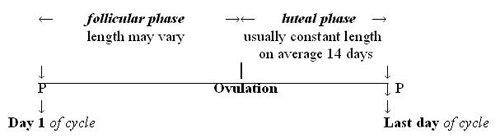
Fig. 6-3; (i) Does ovulation occur at the same time in every cycle; (ii) The two phases of the cycle are not equal in length: The day of ovulation is not fixed in the middle of the cycle but can vary from one cycle to another. It usually occurs about 14 days before the next period. This is because the luteal phase after ovulation has a relatively constant length of 14 days, (range 10-16 days). [e.g. If the cycle length is 30 days, ovulation probably occurred on Day 16 of the cycle (30 minus 14 = 16), and if the cycle length is 25 days, ovulation would probably have occurred on Day 11 of the cycle, (25 minus 14 = 11)]. This means that if the woman’s menstrual cycle is longer or shorter than usual it is the change in length of the follicular phase which causes the longer or shorter cycle.
Hormone secretion in the ovary during the cycle, see Fig. 6-4.
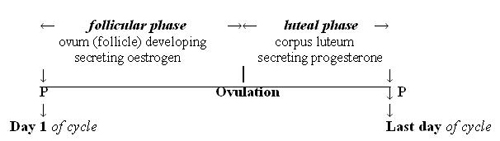
Fig. 6-4; Hormone secretion in the ovary during the phases of the cycle: During the menstrual cycle two steroid hormones are secreted in the ovary, (i) oestrogen by the growing follicle before ovulation and after ovulation (ii) progesterone is secreted by the corpus luteum.
OVERVIEW OF THE PHASES OF THE MENSTRUAL CYCLE (Fig. 6-5)
The two phases of the menstrual cycle, i.e. the follicular phase and the luteal phase, are separated by ovulation.
- Follicular Phase (pre-ovulatory phase): The cycle begins when the pituitary gland releases follicle stimulating hormone (FSH) into the bloodstream. This stimulates a few primordial follicles containing the immature ova in the ovaries to grow, hence the term ‘follicular’ phase. One follicle continues to grow, becomes dominant, and the others regress. The mature follicle is called the Graafian follicle and consists of the ovum surrounded by follicular fluid. The growing follicle secretes oestrogen, which (a) stimulates the endometrium to grow and (b) stimulates the glands of the cervix to secrete mucus necessary for sperm transport and survival.
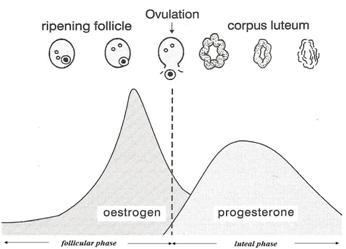
Fig.6-5; Overview of the phases of the cycle: There are a few ripening follicles in the ovary and one becomes dominant, and is released as a mature ovum at ovulation. In the follicular phase of the cycle the oestrogen level in the blood rises as it is secreted by the developing follicle in the ovary before ovulation. When the oestrogen level is high it stimulates the secretion of luteinizing hormone (LH surge) from the pituitary gland see Fig 6-7, The HPO Axis . LH stimulates the mature follicle (Graafian follicle) in the ovary to rupture and the ovum is released into the fallopian tube (ovulation). In the luteal phase of the cycle after ovulation the progesterone level in the blood is high as it is secreted by the corpus luteum. (only the corpus luteum and not the ovary is shown in the luteal phase of the diagram). (Fig. 6-5 from the Fertility Education Trust UK, 2003, is used with the kind permission of Colleen Norman).
- OVULATION: When the Graafian follicle has reached its maximum size it ruptures, releasing the mature ovum into the outer end of the fallopian tube. This event is called ovulation and is triggered by the luteinizing hormone (LH surge) from the pituitary gland. The ovum lives for just 24 hours after it is released. Fertilization takes place in the outer end of the fallopian tube and implantation occurs seven days later in the endometrium. see Figs 6-15 – 6-18 Pages 15,16 in Pictures & Diagrams
- LUTEAL PHASE (post-ovulatory phase): After ovulation the ruptured follicle in the ovary becomes a small gland called the corpus luteum (yellow body) which secretes both progesterone and oestrogen. Progesterone maintains the integrity of the endometrium. The corpus luteum has a finite life of about 14 days and this means that the luteal phase has a relatively constant length of 14 days, (range 10-16 days). Progesterone reaches its highest level seven days after ovulation and if the ovum has not been fertilized the corpus luteum will then start to regress causing a marked drop in progesterone level. Following this the endometrium can no longer be maintained and is shed as menstruation about 14 days after ovulation. A new cycle then begins.
References:
- Brown JB; ‘Types of ovarian activity in women and their significance: the continuum (a reinterpretation of earlier findings’); Human Reproduction Update; vol 17; No 2; p141-158. (this is a classic article which gives a greater understanding of the menstrual cycle throughout the reproductive life.)